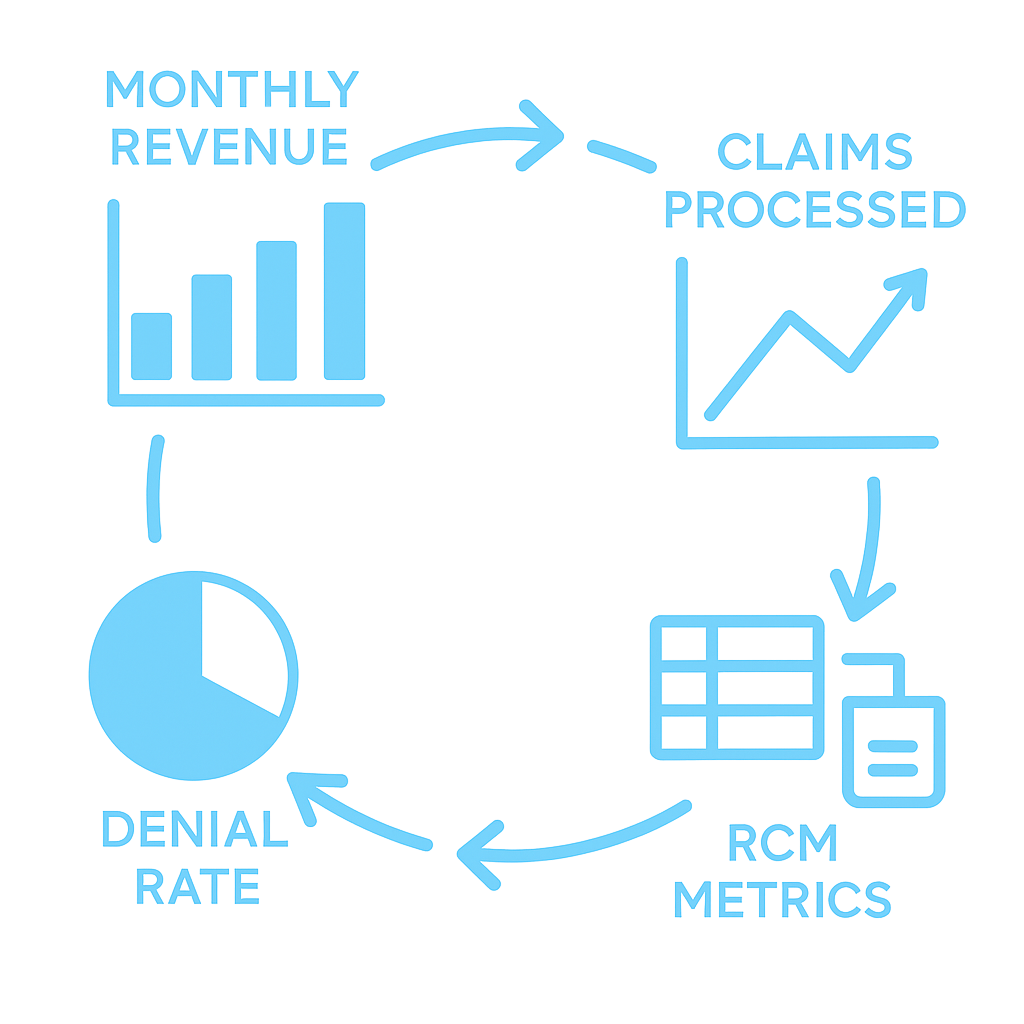
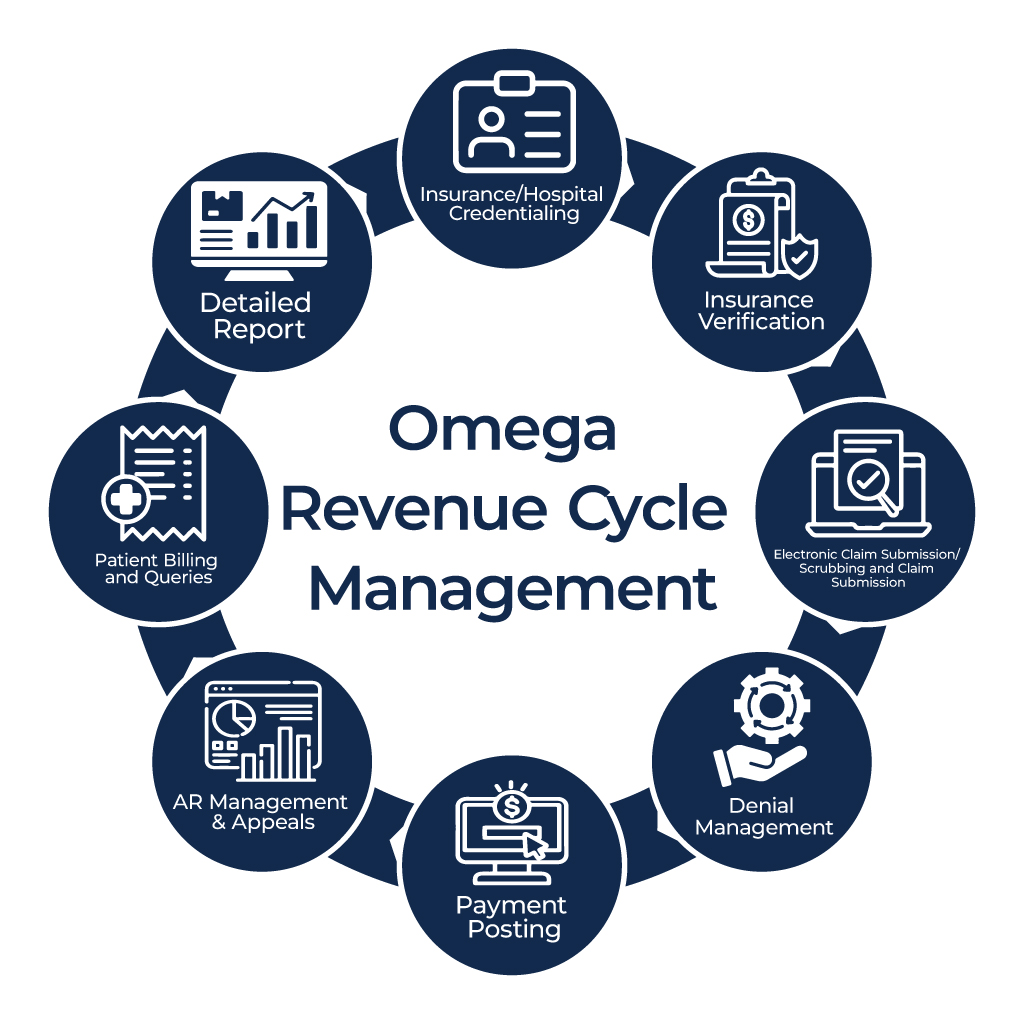
Omega Medical Billing offers comprehensive, end-to-end billing solutions,
including credentialing, accurate coding (CPT & ICD-10), clean claim
submissions, denial management, and detailed performance reporting. We also
manage your complete billing cycle, ensuring timely payments and a steady
revenue flow. Additionally, our services include benefits verification and
eligibility checks, allowing you to confirm patient coverage and streamline the
claims process for improved accuracy and reduced denials.